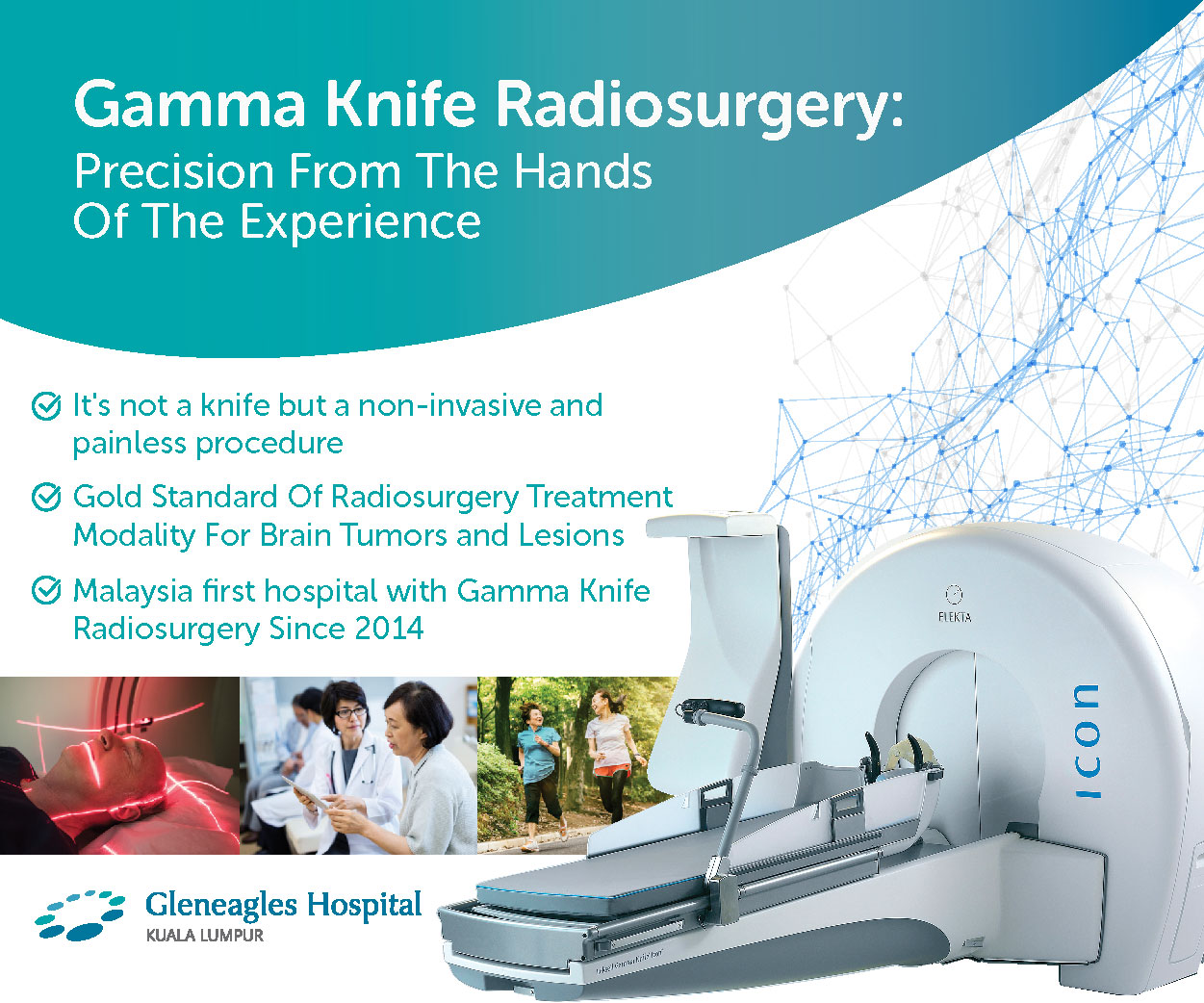
The gold standard in radiosurgery treatment of brain tumours and lesions
Benefits include faster set-up and treatment delivery to multiple tumours in a single session, and the potential to treat lesions in areas not able to be reached by older models, including tumours in the sinuses, orbits, and upper cervical spine. Icon™ allows treatments of a wider range of targets faster and more efficiently than ever before.
The radiosurgery system’s unique radiation-focusing device ensures superior
radiation delivery and accuracy while reducing the dose to unintended areas. Icon™
is fine-tuned to the task, resulting in fast, and efficient treatments.
Gamma Knife is a non-invasive neurosurgical procedure which uses powerful doses of radiation to target and treat diseased brain tissue while leaving surrounding tissue intact. There is no real knife involved, rather the ‘knife’ refers to 192 precise beams of radiation that attack tumours and abnormalities, shrinking them over time or stopping their growth.
No incisions are made in the patient’s head, instead very precisely focused beams of radiation are directed to the treatment area in the brain. This groundbreaking technology allows physicians to operate on brain lesions often considered inoperable; offering new hope for patients with brain tumours, vascular malformations and functional disorders.
Gamma Knife surgery safely and effectively treats over 70,000 patients every year. The treatment procedure is simple, painless and straightforward.
- Precision Treatment : Treatment is directed at targeted areas only, preserving healthy tissue.
- Better Outcome : Reaches areas that traditional brain surgery cannot.
- Safer : Compared to traditional brain surgery.
- Less Complication: No scalpel or other surgical tools are used – low risk to surrounding tissue
- Quick Recovery : Same-day discharge after treatment
- Non-Invasive : No opening of the skull or shaving of the head
- No Pain : Bloodless, virtually painless
Gamma Knife Surgery is usually performed when:
- A tumor or other abnormality in the brain is too hard to reach with standard neurosurgery
- A patient isn't healthy enough to undergo standard surgery
- A patient prefers a less invasive treatment
Gamma Knife radiosurgery is commonly used to treat the following conditions:
- Brain tumor - small noncancerous (benign) and cancerous (malignant) brain tumors
- Arteriovenous malformation (AVM)
- Trigeminal neuralgia
- Acoustic neuroma
- Pituitary tumors
My Brain Journey through Gamma Knife Surgery : Painless, Precise and Effective.
Video:
(https://www.facebook.com/gleneagleskualalumpur/videos/463561874804000)
(https://www.facebook.com/gleneagleskualalumpur/videos/2609782005910930)
Conditions for which the Gamma Knife is considered are:
- Malignant tumors such as metastases (cancer that has spread to the brain) and malignant gliomas
- Benign tumors such as meningiomas, acoustic neuromas (vestibular schwannomas), pituitary tumors and low grade glioma and skull-based tumors
- Vascular malformations such as arteriovenous malformations (AVMs) and cavernous angiomas (cavernous malformations)
- Functional disorders such as trigeminal neuralgia
Gamma Knife radiosurgery is especially valuable for patients whose neurological disorders require a difficult surgical approach or may be impossible to treat using conventional neurosurgical techniques. Patients of advanced age or in poor medical condition can be at an unacceptably high risk for anesthesia and conventional surgery, making Gamma Knife treatment an ideal solution.
Gamma Knife technology also is highly beneficial for patients whose lesions are situated in an inaccessible or functionally critical area within the brain. In addition, the treatment can be used as an adjunct to the care of a patient who has undergone conventional brain surgery, interventional neuroradiology or conventional radiation therapy or chemotherapy.
The Gamma Knife’s success rate is impressive. Supported by more than two decades of clinical research and over 700,000 procedures done worldwide, this neurosurgical tool has met with unprecedented results. Clinical applications continue to grow, and its many benefits as a non-invasive treatment modality continue to make it the treatment of choice for certain clinical conditions.
Once a patient’s condition is reviewed by our multidisciplinary team and Gamma Knife treatment is deemed appropriate, the patient will be scheduled for a treatment day. On the day of treatment, there are several steps that take place. First, a lightweight frame is attached to the patient’s head. Local anesthesia is used before the frame is secured in place. The patient then has an MRI or CT imaging study, or in the case of an arteriovenous malformation, angiography, may be needed in order to precisely locate the diseased area. Data from the imaging study is transferred into the treatment planning computer. While the patient rests, the treatment team (a neurosurgeon, radiation oncologist and physicist) uses advanced software to determine the treatment plan. This takes one or two hours to complete, depending on the complexity and location of the disease.
When the individual treatment plan is completed, the patient is placed on the Gamma Knife couch and precisely positioned. The patient is then moved automatically, head first into the machine, and treatment begins. Treatment typically lasts from 15 minutes to an hour or more, during which time the patient feels nothing unusual.
Actual treatment time varies based on the condition being treated and its location. Following treatment, the patient is automatically moved out of the machine, and the head frame is removed.
During the actual procedure, the patient does not see or feel the radiation during treatment. Before the treatment takes place, patients typically feel slight discomfort from the local anesthetic used prior to head frame placement and have reported feeling pressure for a short time while the pins are inserted to fixate the head frame, but no pain.
The patient remains conscious throughout the entire procedure and may communicate with the treatment team.
No, the head is not shaved. In rare cases the treatment may cause some hair loss.
When the treatment is finished, the head frame will be removed. Sometimes there is a little bleeding from where the pins were attached to the head. In this case, gauze and pressure will be applied to stop the bleeding and keep the area clean. A temporary head dressing is placed to keep the pin sites clean. It is recommended that the patient take it easy over the next 12 to 24 hours. Pre-Gamma Knife activities can be resumed within a few days.
The Gamma Knife allows non-invasive brain surgery to be performed with extreme precision while sparing healthy tissues surrounding the targeted treatment area. Also, because neither a surgical incision nor general anesthesia is required, the risks usually involved with open brain surgery, such as hemorrhage or infection, may be reduced. Hospitalization is rarely required and recovery time is minimal. While individual patient outcomes may vary, patients may resume their normal pre-surgery lifestyle within a few days.
You may bring music to listen to during your treatment. We can accommodate iPods or CDs. As there is limited room, only one to two family members can be with you at a time prior to your treatment. Please keep all valuables at home.
If you have any questions or for enquiries on our Gamma Knife Promotional Package, please contact the Gamma Knife Resource Centre at +603 4141 3091 or +603 4141 3528 or +603 4141 3530













-500x500.webp?sfvrsn=60351b85_7)
















